Introduction
Ultrasound phantoms can cost upwards of $700 (source). This is a steep price for students, educators, or clinicians who simply want to practice their technique. I wanted to create a low-cost alternative that would let me rehearse ultrasound-guided peripheral IV (PIV) placement without breaking the bank.
While reviewing organic chemistry, I started thinking about polymers and remembered Mary Roach’s Stiff: The Curious Lives of Human Cadavers mentioning ballistic gel. Ballistic gel is a synthetic or gelatin-based material originally developed to replicate the density and viscosity of human tissue for projectile impact testing. That made me wonder if it could mimic the echogenicity of expensive phantoms like the CAE Blue Phantom.
Come to find, many others came to the same conclusion, so there is a wealth of info online about making these low cost alternatives.
Armed with that insight, I decided to start experimenting. My goal wasn’t perfection, but progress: to build something functional, testable, and cheap. Each attempt became a prototype, teaching me something new about materials, design, and the trade-offs between realism, durability, and ultrasound performance. Here’s a breakdown of what I tried, what worked, and what didn’t.
Prototype 1
For my first attempt, I used 20% NATO ballistic gel produced from a low cost ballistic gel alternative from Fit Lane Nutrition/Amazon and opted for silicone tubing instead of latex. I had come across a tip on 5MinSono noting that latex tubing can shrivel when exposed to hot gel before it set.
I used an ice mold for shaping, which was easy and accessible, but I made the phantom nearly 2 inches (5.08 centimeters) thick. That turned out to be a major misstep and far too deep for realistic PIV insertion practice. In real patients, superficial veins are usually within 0.5 to 1 cm of the skin surface, so this block made even shallow access feel like a central line attempt.
Still, it was a useful baseline to learn from, especially about material behavior and the importance of scale in procedural realism.
Prototype 2
For the second attempt, I went with a 10% FBI ballistic gel mix and poured it into a bread pan, creating a block about 1.5 inches thick. The size and shape worked somewhat better but the depth was barely acceptable for practicing superficial vein access.
Functionally, it was solid for basic training, but the “mock tissue” lacked echogenicity. The gel appeared mostly anechoic, making it difficult to appreciate needle depth or surrounding structures on ultrasound. To improve vessel visualization, I injected saline into the vein cavity. Without it, the air-filled veins showed up like bright fog lights—far too echogenic for realistic image interpretation.
One major drawback is that the block sheared apart after just one or two attempts. The lower gel concentration made it soft and fragile. However, ambient temperature may have also played a role. The room was warm, and the gel felt noticeably softer than when it had first set, suggesting that even small temperature shifts could affect its mechanical stability. This made the block less forgiving to needle passes and more prone to tearing with repeated use.
Prototype 3
For this iteration, I went with a smaller form factor and re-melted my original 20% NATO block. This time, I incorporated cornstarch at a 10% concentration to increase echogenicity in the surrounding “tissue” (source). The goal was to make the phantom appear more realistic under ultrasound, with improved scatter and soft tissue texture. It worked, and the structures looked more like actual tissue, and the needle was easy to track on screen as it pierced and advanced through the gel.
That realism came at a cost. The block lost its translucency. In earlier versions, I could visually track the needle as it approached the vein, which helped correlate hand motion with needle tip position. With the added echogenicity, that visibility disappeared. It’s a trade-off: better imaging fidelity on the screen, but less direct visual feedback.
One additional observation: the added density made it more difficult to fully compress the mock vein with the probe. While this might not perfectly simulate real-world vein behavior, it didn’t seem to hinder needle guidance. Overall, this version struck a better balance between ultrasound realism and practical usability.
Comparisons
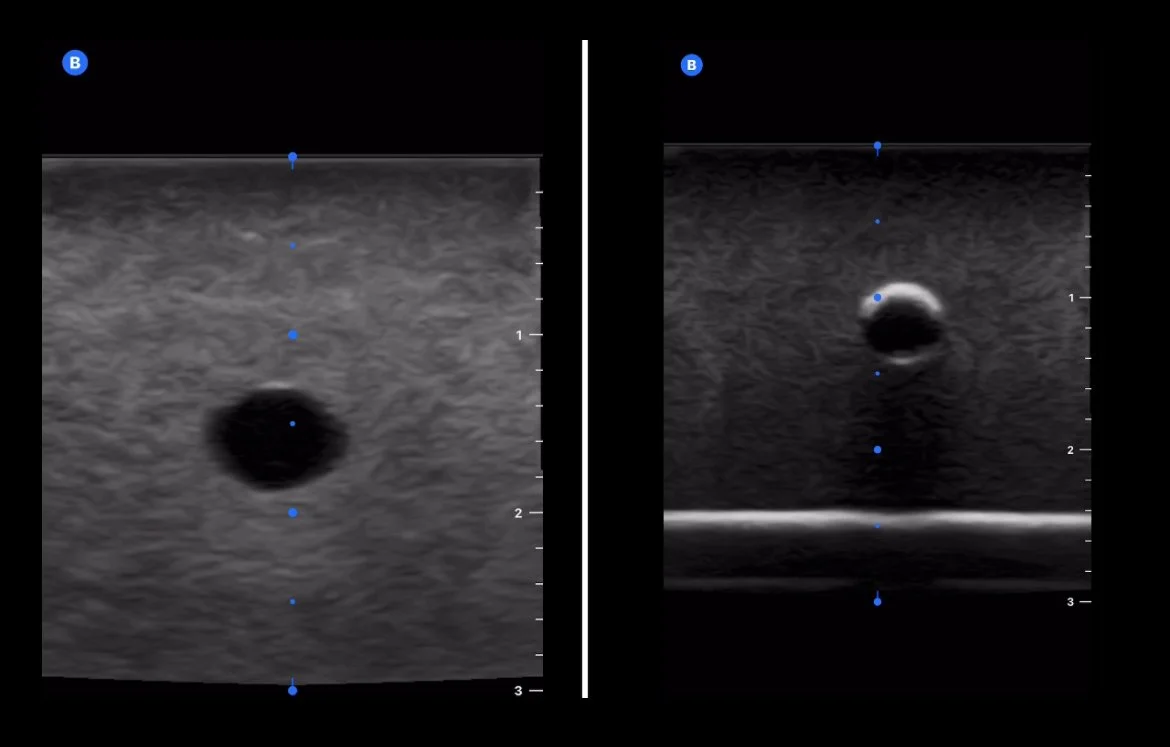
Prototype 2 (left) via Mindray versus Prototype 1 (right) via Butterfly.
Left is a $500 US phantom from a medical simulation company. Right is Prototype 2, which comes in at approximately $10.
Future Considerations
The bargain-brand ballistic gel I used for these prototypes is made from organic gelatin, most likely bovine in origin. While affordable and easy to work with, this type of gel isn’t truly shelf-stable. It can degrade, soften, or even grow mold over time when stored at room temperature. For short-term use or small batch experimentation, it works well. But for long-term durability and reusability, I’m looking into synthetic alternatives.
These synthetic gels come with a higher upfront cost for raw materials, but they’re still significantly cheaper than commercial medical training models. They’re also more stable, reusable, and less prone to biological breakdown. In future iterations, I also plan to experiment with graphite powder instead of cornstarch as my echogenicity agent. Graphite offers a more consistent ultrasound appearance and, importantly, it doesn’t support microbial growth, making it a better choice for models intended to last.